Written by Bianca Maria Borrelli & Christos Tsagkaris
Introduction
The Cancer of the cervix Uteri or Cervical Cancer (CC) or is defined as an abnormal proliferation of mutated cells in the internal lining of the cervix, the segment that connects the body of the Uterus with the Vagina (1)
Nowadays in Italy and worldwide it is the second most common cancer in females with almost 3700 new cases diagnosed annually in Italy and 570000 new cases worldwide in 2018 (2,3). These figures confirm its role as an important global and public health issue. The major cause of the malignant transformation of the cells is being infected with HPV virus’ specific subtypes, widely known as high risk serotypes (4,5). A persistent infection from HPV viruses can causein due time a malignant transformation of the infected cells. The oncogenic potential of the virus is a result of its effort to replicate within the infected cells altering their DNA (10).
Being aware of the cancerous effect of HPV we are able to prevent or detect CC early.
On these grounds, the Public Institutions of Health offer programs of prevention to fight against the spread of this disease (13).
Primordial, Primary and Secondary Prevention
Primordial prevention consists of promoting lifestyle changes at a population level. As vague as it may seems, primordial prevention in the case of HPV can be realized through education and dissemination of evidence based protection measures such as the use of condoms. Primary prevention is the first step of the screening programs aiming to protect people from contracting the disease.The second step is what we call secondary prevention, which means testing non-symptomatic people in order to discover as soon as possible the presence of the disease and act an early treatment that has the best chance to be effective.
Screening Programs in the frame of Primary Prevention
Primary prevention for cervical cancer is synonymous with HPV vaccination. Recent evidence suggests that vaccinating both females and males decreases significantly the possibility of contracting the disease and developing cancer. (6 – 8).
HPV is the most common sexually transmitted virus that can infect both male and female, generating an asymptomatic infection (6). Contrary to what one might think, this is actually a negative aspect, because the absence of any symptom means that the chance to transmit the disease increases since people are not aware whether they are carriers transmitting the virus or not. In Italy the vaccination is offered for free from the Italian National Health Care Association to all the adolescents of 11-12 years old and it’s highly recommended (11).
Screening Program in the frame of Secondary Prevention
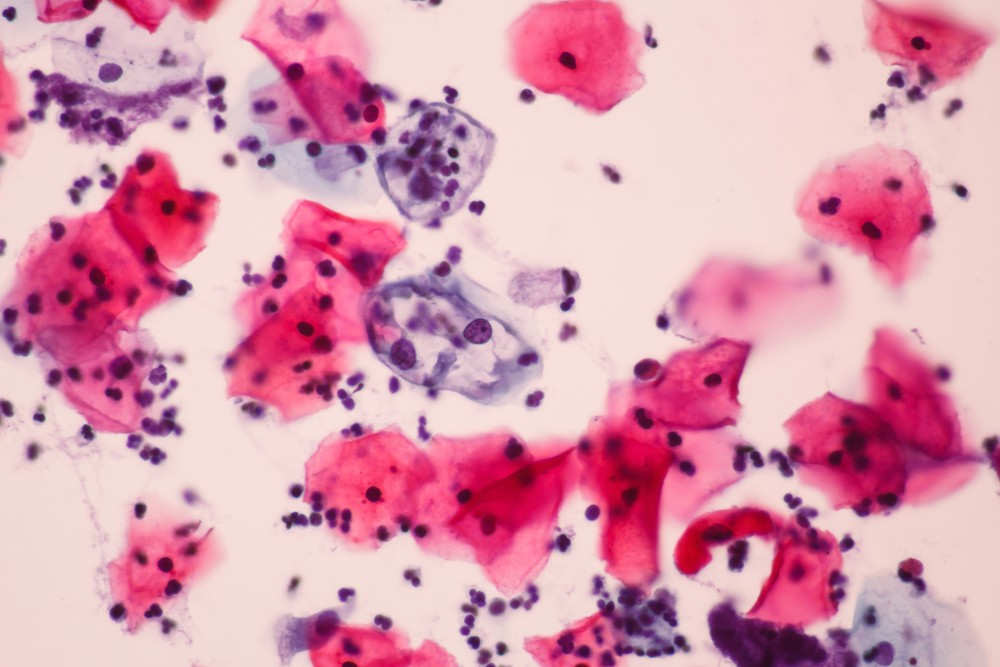
Secondary prevention measures provide the possibility to detect and treat the disease at an early stage of development. A microscopic examination of genital smear followed by a simple surgical procedure if the findings are compatible with malformation, can eradicate the lesion, cure the disease and achieve the optimal outcome (1).
Two strategies are suggested by the Italian National screening programs: the Pap Test (6) and the HPV test (12). They are offered to healthy women without symptoms because having no symptoms doesn’t mean having no disease (1). Usually, the symptoms correlated to cervical cells’ abnormal proliferation appear only when the disease is advanced or has already spread in the body (1).
The Pap Test consists of taking a sample of the cervix’s cells wall through a simple exfoliation with a vaginal swab and examining them searching for morphological abnormalities. This screening test is offered and recommended to all the women between the age of 25-64 years and should be repeated every 3 years (13).
The HPV Test is a molecular test capable of detecting the high-risk-serotype HPV viruses’ DNA in the cervical cells (12).
The sample is obtained in a similar way to the Pap Test. Finding the viral DNA means that the cells have been infected with the dangerous HPV viruses serotype and further examinations should be done (14).
In Italy the screening with the HPV Test is initiated at the age of 30 until 65 years for all the women, and should be repeated every 5 years (13).
These time schedules are facilitated by the Italian National Health Care Association with the purpose of designing the best screening strategy possible in order to reach the best proportion between risk and benefit and to avoid unnecessary medical intervention.
Of course both screening tests cannot offer total protection from developing cancer. There is always a risk. However, abiding by these suggestions minimizes the risk. And this has been suggested by evidence based studies and is still being established in contemporary clinical practice. Equally, the HPV vaccination cannot protect from all the high risk HPV infections and doesn’t protect from a previous contact with the virus. Getting vaccinated doesn’t mean that there is no more need of the secondary tests.Vaccination provides immunity against the most common dangerous serotypes of HPV, however there is the possibility to contract another dangerous oncogenic serotype (6).
Thanks to the introduction of these tests, the mortality rate for cervical cancer has drastically fallen down in the last years (9). Apparently, more cases were diagnosed with an increase in the prevalence, but actually this rise is justified from the improvement of the sensitivity with which we detect the disease.. We are now diagnosing all the cases that we would have otherwise diagnosed later, in a more aggravated and hence more life-threatening form
Conclusions
In the previous years, lack of information and false alarms about vaccination and secondary prevention tests has generated an incomplete adhesion of the population to the recommended screening schedule, leaving the need to raise the general awareness about these important topics. Taking part in the prevention programs offered by the National Health Care Associations means the world in terms of public health and in terms of personal wellbeing. Nowadays, the European Union as a whole as well as its member states are taking important steps to tackle cancer. Paneuropean state organizations such as the Health and Food Safety authorities and civil society entities such as the Association of European Cancer Leagues, national and regional institutions have joined forces to decrease the number of cancer patients by 50% in the proximal future.. A future free of cancer can be possible, and cervical cancer is expected to be one of the first neoplasms to be eliminated. But it takes a lot of work in science, a lot of persuasion in policy and a lot of effort in society.
References
“Cervical Cancer Treatment (PDQ®)”. National Cancer Institute. 2014-03-14. Archived from the original on 5 July 2014. Retrieved 25 June 2014.
AIOM, I numeri del cancro in Italia 2017, Il pensiero scientifico editore (archiviato dall’originale).
World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 5.12.
Kumar V, Abbas AK, Fausto N, Mitchell RN (2007). Robbins Basic Pathology (8th ed.). Saunders Elsevier. pp. 718–721
Kufe, Donald (2009). Holland-Frei cancer medicine (8th ed.). New York: McGraw-Hill Medical. p. 1299. ISBN9781607950141. Archived from the original on 2015-12-01.
“Human Papillomavirus (HPV) Vaccines”. National Cancer Institute. 2011-12-29. Archived from the original on 4 July 2014. Retrieved 25 June 2014.
“FDA approves Gardasil 9 for prevention of certain cancers caused by five additional types of HPV”. U.S. Food and Drug Administration. 10 December 2014. Archived from the original on 10 January 2015. Retrieved 8 March 2015.
Tran, NP; Hung, CF; Roden, R; Wu, TC (2014). Control of HPV infection and related cancer through vaccination. Recent Results in Cancer Research. 193. pp. 149–71
Canavan TP, Doshi NR (March 2000). “Cervical cancer”. American Family Physician. 61 (5): 1369–76. PMID10735343. Archived from the original on 2005-02-06.
Gadducci A, Barsotti C, Cosio S, Domenici L, Riccardo Genazzani A (August 2011). “Smoking habit, immune suppression, oral contraceptive use, and hormone replacement therapy use and cervical carcinogenesis: a review of the literature”. Gynecological Endocrinology. 27 (8): 597–604
Cervical cancer screening in Europe: Quality assurance and organisation of programmes. Elfström KM, Arnheim-Dahlström L, von Karsa L, Dillner J Eur J Cancer. 2015 May; 51(8):950-68.
Evidence regarding human papillomavirus testing in secondary prevention of cervical cancer. Arbyn M, Ronco G, Anttila A, Meijer CJ, Poljak M, Ogilvie G, Koliopoulos G, Naucler P, Sankaranarayanan R, Peto J Vaccine. 2012 Nov 20; 30 Suppl 5():F88-99.
British Journal of Cancer (2004) 91, 935 – 941& 2004 Cancer Research UK All rights reserved 0007 – 0920/04
HPV-FASTER: broadening the scope for prevention of HPV-related cancer.Bosch FX, Robles C, Díaz M, Arbyn M, Baussano I, Clavel C, Ronco G, Dillner J, Lehtinen M, Petry KU, Poljak M, Kjaer SK, Meijer CJ, Garland SM, Salmerón J, Castellsagué X, Bruni L, de Sanjosé S, Cuzick J
Nat Rev Clin Oncol. 2016 Feb; 13(2):119-32.

 Unity and Disunity in EU Diplomacy: Why Speaking with One Voice Remains Difficult
Unity and Disunity in EU Diplomacy: Why Speaking with One Voice Remains Difficult  Sharing the Costs of Climate Ambition: Rethinking Justice in the EU’s CBAM
Sharing the Costs of Climate Ambition: Rethinking Justice in the EU’s CBAM  The ’Ndrangheta’s Infiltration and Threat to European Institutions
The ’Ndrangheta’s Infiltration and Threat to European Institutions  From Paper to Practice: How Grassroots Norms Undermine Gender Rights in Pakistan
From Paper to Practice: How Grassroots Norms Undermine Gender Rights in Pakistan